Vascular Health · Vein Disease
So… What Are Those Venous Insufficiency Symptoms Your Legs Keep Showing You?
Vein Disease in Legs · Blood Pooling · Treatment Options 2026
Most people do not notice it arriving. The legs feel heavier than usual. The ankles are a little puffier by evening. You put it down to a long day. But when those feelings become your new normal, something deeper is happening inside your veins. And it has a name.

Venous insufficiency affects millions of people, often progressing silently over years before symptoms become severe.
What Is Venous Insufficiency?
Venous insufficiency is a condition in which the veins in your legs can no longer efficiently return blood to the heart. Inside every healthy vein, tiny one-way valves open to allow blood to travel upward and snap shut to prevent it sliding back down. When those valves weaken, wear out, or become damaged, they lose their ability to seal properly. Blood begins traveling backward and collecting in the lower legs, a process known as blood pooling in legs.
That pooling is not just an inconvenience. Over time, it raises pressure inside the vein walls, stretches the vessels, starves surrounding tissue of oxygen, and triggers a cascade of venous insufficiency symptoms that become increasingly difficult to ignore, and increasingly damaging if left unaddressed.
"Venous insufficiency is not a dramatic condition. It creeps in quietly, through aching legs, stubborn swelling, and skin that slowly changes. By the time most people take it seriously, it has already been building for years."
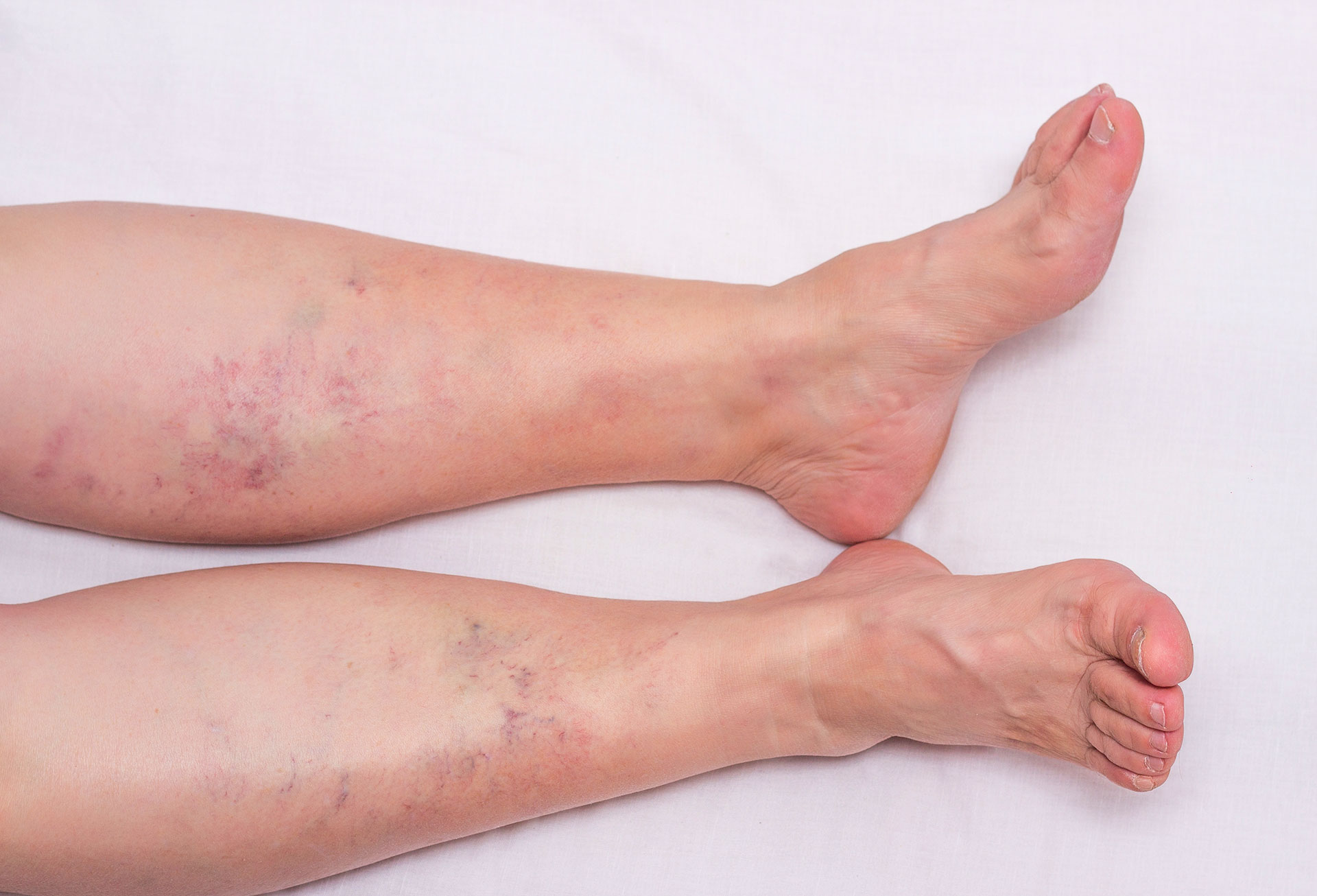
Swelling, skin discoloration, and visible veins are among the most recognizable signs of vein disease in legs.
Why Vein Disease in Legs Develops
Vein disease in legs does not appear overnight. It develops gradually, driven by a combination of inherited vulnerability and everyday lifestyle factors. The single biggest contributor is damaged vein valves, but several forces determine who is most at risk and how quickly the condition progresses.
Risk Factors Behind Venous Insufficiency
Family HistoryThe structure and resilience of vein walls and valves is largely inherited. If a parent or sibling has venous insufficiency or varicose veins, your own risk is meaningfully higher.
Prolonged Standing or SittingWhen you remain stationary for long periods, the calf muscles that normally help pump blood upward become inactive. Venous pressure rises steadily, and over years this erodes valve function.
PregnancyHormonal shifts and increased blood volume place extra stress on vein valves. Many women notice the first signs of vein disease in legs during or shortly after pregnancy.
Prior Deep Vein Thrombosis (DVT)A past blood clot in the deep veins of the calf or thigh can permanently scar vein valves, triggering venous insufficiency legs years after the clot itself has resolved.
Excess Body WeightAdded mechanical pressure on the venous return system forces valves to work harder over time, speeding up their deterioration.
SmokingNicotine damages vessel walls and impairs circulation, contributing to both vein wall weakness and valve failure.
Low Physical ActivityThe calf muscles act as the primary venous pump in the legs. A sedentary lifestyle eliminates this mechanism and allows blood pooling in legs to worsen progressively.
PhlebitisInflammation of a superficial vein causes scarring that reduces the vessel's ability to carry blood efficiently, contributing to venous insufficiency over time.
Recognizing Venous Insufficiency Symptoms
The frustrating reality of venous insufficiency symptoms is how easy they are to dismiss. Tired legs. A little ankle puffiness. Skin that itches for no obvious reason. Each sign on its own seems minor. Together, they form a pattern that a vascular specialist recognizes immediately.
Warning Signs to Watch For
Leg Heaviness and Persistent AchingA disproportionate tiredness in the calves and thighs, especially after standing or sitting for long periods. This is typically the earliest venous insufficiency symptom people notice.
Swelling in the Lower Legs and AnklesAs blood pooling in legs raises venous pressure, fluid is forced out of the vein walls into surrounding tissue. Swelling worsens throughout the day and typically improves with overnight elevation.
Itching, Burning, or Tightness in the CalvesInflammation in the skin and tissue overlying congested veins causes chronic irritation. This is a common early sign that venous insufficiency legs are not receiving adequate circulation.
Skin Discoloration Near the AnkleA brownish or reddish staining develops when red blood cells leak out of overpressured veins and break down in surrounding tissue (a condition called lipodermatosclerosis). This signals significant, sustained venous pressure.
Varicose VeinsEnlarged, bulging, ropey vessels visible at the skin surface are among the most recognizable manifestations of vein disease in legs, and a clear sign the venous system is under serious strain.
Restless Legs and Night CrampsAn uncomfortable urge to move the legs, or sudden painful muscle spasms during sleep, are frequently linked to venous insufficiency rather than muscular or neurological causes.
Pain That Improves With Rest or ElevationLeg discomfort that eases when you sit, lie back, or raise your legs above heart level is a hallmark pattern of venous origin pain, distinguishing it from arterial or musculoskeletal conditions.
Venous Leg UlcersThe most serious consequence of untreated venous insufficiency. Open, slow-healing wounds that typically form near the ankle require specialist management and will not resolve without addressing the underlying blood pooling in legs.
Many venous insufficiency symptoms overlap with other conditions. A confirmed diagnosis from a vascular specialist, including a duplex ultrasound, is the only reliable way to identify venous insufficiency and rule out other causes.
How Venous Insufficiency Is Diagnosed
A vascular specialist will begin with a detailed review of your medical history and a physical examination of your legs. The definitive diagnostic tool is a duplex ultrasound, a non-invasive imaging scan that maps blood flow direction and speed inside your veins in real time.
Duplex Ultrasound: The Definitive Test
The duplex ultrasound identifies exactly which valves are failing, measures how severely blood is refluxing backward, distinguishes between superficial and deep venous insufficiency, and rules out deep vein thrombosis as a contributing cause. It is painless, takes around 30 to 45 minutes, and provides the precise information needed to build a personalized treatment plan.
"A duplex ultrasound does in 30 minutes what years of symptom-watching cannot: it shows exactly where the vein valves are failing and how severely blood is pooling in the legs."
Treating Venous Insufficiency Legs: Your Options
Modern treatment for venous insufficiency is considerably less invasive than it was even a decade ago. The right approach depends on how advanced the vein disease in legs has become, your overall health, and your goals. In most cases, meaningful and lasting relief is achievable.
Compression Therapy and Lifestyle AdjustmentsGraduated compression stockings apply controlled external pressure to the legs, reducing swelling and supporting venous return. Combined with regular walking, leg elevation, weight management, and movement breaks, they can significantly slow blood pooling in legs and ease daily venous insufficiency symptoms. For mild cases, this combination may be sufficient.
SclerotherapyA specialist injects a solution directly into the affected vein, causing its walls to scar and seal permanently. Blood naturally reroutes through nearby healthy vessels. Sclerotherapy is the gold standard for spider veins and small-to-medium varicose veins, with visible results typically appearing within three to six weeks.
Endovenous Laser Ablation (EVLA) and Radiofrequency Ablation (RFA)A thin catheter is guided into the diseased vein under ultrasound guidance. Thermal energy delivered from inside seals the vessel shut and redirects blood flow to healthy veins. Minimally invasive, highly effective for larger veins, and most patients return to normal activity the same day.
VenaSeal Closure SystemA medical-grade adhesive is injected to permanently seal the diseased vein: no heat, no tumescent anesthesia, minimal post-procedure bruising. One of the most comfortable and effective treatments currently available for venous insufficiency legs, including chronic venous insufficiency causing persistent blood pooling in legs.
Surgical Options (Ligation and Stripping)Reserved for advanced vein disease in legs where minimally invasive approaches are insufficient. Ligation ties off the affected vein to eliminate blood flow through it. Stripping physically removes heavily damaged veins. Both are performed under anesthesia and carry longer recovery periods than non-surgical alternatives.
When to See a Vascular Specialist
Do not wait for a venous ulcer before you seek help. If you are experiencing any combination of the venous insufficiency symptoms described above, including persistent leg heaviness, swelling that returns daily, skin changes near the ankle, visible varicose veins, or night cramps, a consultation with a vascular specialist is the right next step.
Early intervention in vein disease in legs prevents the condition from advancing, protects your long-term mobility, and in most cases resolves symptoms quickly and durably. A duplex ultrasound is all it takes to understand exactly what is happening inside your veins and what your best path forward looks like.

Modern treatments for venous insufficiency are minimally invasive, effective, and require little to no recovery time.
"The earlier venous insufficiency is addressed, the simpler the treatment and the better the outcome. Waiting only narrows your options."

